Home
What is Dystonia?
Dystonia is a neurological movement disorder which may affect anyone at any age. It is characterised by involuntary muscle contractions which force certain parts of the body into abnormal, sometimes painful, movements or postures. Dystonia can affect any part of the body including the arms and legs, trunk, neck, eyelids, face, or vocal cords.
Latest News
Keep up to date with all that's happening at Dystonia Ireland.
Get Rare Aware campaign
By Dystonia Ireland |
Thanks to everyone (35 organisations this year!) for your support of the upcoming Get Rare Aware campaign, launching next week. A few asks for you. We need patient voices for…
Read More VHI Womens’ Mini Marathon 2024
By Dystonia Ireland |
This year the VHI Womens Mini Marathon will take place on Bank Holiday Sunday 2nd June 2024. We would love to have you join us on the day for Dystonia Ireland and…
Read More Rare Disease Day
By Dystonia Ireland |
Rare Disease Day is the globally-coordinated movement on rare diseases, working towards equity in social opportunity, healthcare, and access to diagnosis and therapies for people living with a rare disease.…
Read More Recovery Rising Cycle For Dystonia Ireland
By Dystonia Ireland |
Thanks to Catriona Nally for organising this fundraising event in aid of Dystonia Ireland. The Cycle takes place on August 27th, from Ballymun to Tiglin, Greystones. Find out more and…
Read More Charity Soccer Tournament in Aid of Dystonia Ireland On July 23rd 2023
By Dystonia Ireland |
Thanks to Darcy O Sullivan and his friends for raising €3,100 for Dystonia Ireland at this event. Read more about the event at: https://m.independent.ie/regionals/kerry/tralee-news/photos-show-tralee-bar-and-hotel-staff-enjoying-charity-soccer-tournament-for-dystonia-ireland/a788354191.html — Darren (Darcy) O’Sullivan from Tralee…
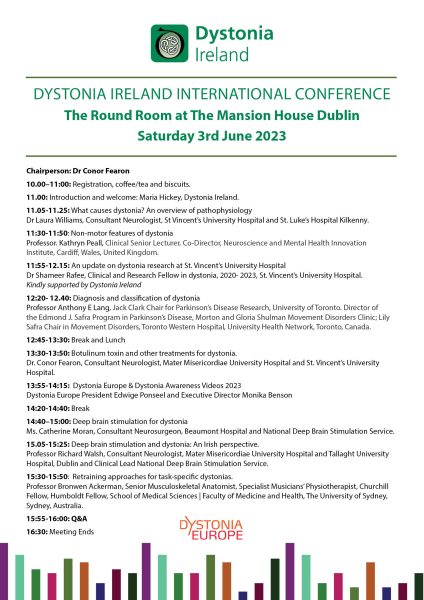
Read More Dystonia Ireland International Conference – 3rd June 2023
By Dystonia Ireland |
++ Still time to register for this event++Tel: 003531 4922514 or E-mail: info@dystonia.ie to register. Dystonia Ireland International Conference: The Round Room at The Mansion House Dublin Saturday 3rd June…
Read More Follow Us
Connect with us on Social Media